Today, such a disease as osteochondrosis of the thoracic and cervical spine is considered a fairly common disease among people of all ages.

A sedentary lifestyle, improper posture and wearing uncomfortable shoes can lead to a rather serious illness, which is almost impossible to diagnose in the initial stages.
Features of osteochondrosis of the thoracic spine
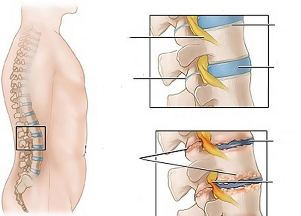
Osteochondrosis of the thoracic spine, most often called thoracic chondrosis, is a disease of the intervertebral discs of the thoracic spine. Also, thoracic degenerative disc disease is called "chameleon", since the symptoms are not detected immediately and can be mistaken for a completely different disease.
Most often, the disease occurs due to metabolic disorders, as well as excessive stress on the intervertebral discs. Thoracic chondrosis disrupts the normal functioning of the intervertebral disc.
Unlike other types, thoracic osteochondrosis is less pronounced and has the following symptoms:
- Aching pain in the chest,worse at night, as well as with sharp turns, or hypothermia.
- Pain between the shoulder bladeswith a sharp rise of the limb, or sharp bends.
- Sharp pain when sighingand chest tightness.
The above symptoms refer to the initial stage of the disease.
With a prolonged course without medical intervention, the following symptoms may appear:
- Numbness in small areas of the skin.
- Itching or burning in the legs.
- Severe flaking of the skin.
- Mild pain in the throat or esophagus.
- Poor gastrointestinal function.
Osteochondrosis of the cervical spine
Osteochondrosis of the cervical spine, or cervical chondrosis, is a disease that weakens the intervertebral discs, leading to a change in the structure of the discs themselves and cervical joints. Nerve endings can become inflamed, being compressed by destructive intervertebral discs.
According to the International Classification of Diseases (ICD-10), it has the M42. 02 code.
The following pain sensations are inherent in the disease:
- Periodic headaches.
- Periodically aching pain in the neck, back, shoulders.
- Short-term visual impairment.
- Decrease in the sensitivity of the collar zone.
Symptoms of cervical chondrosis
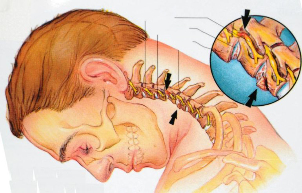
The second degree is characterized by the appearance of small spinal hernias and the following symptoms:
- Pain in the cervical spine, strong crunching on a sharp turn of the head.
- Periodic loss of sensation in the arms and shoulders.
- Visual impairment and recurrent ringing in the ears, trouble sleeping.
- Numbness of the face and neck, weakening of the upper limbs.
- Periodic sharp pain in the shoulder blades.
The third stage of cervical osteochondrosis is difficult to treat. The intervertebral hernia increases in size, there is a deformation of the spine.
For the third stage, the following symptoms will appear:
- Severe pain in the neck and heart.
- Loss of sensitivity on the scalp, arms, shoulders.
- Paralysis of the upper limbs.
- Hernia of the cervical vertebrae.
The fourth stage is characterized by an exacerbation of all of the above symptoms.
Symptoms of cervicothoracic osteochondrosis
A fairly common disease that immediately affects the cervical and thoracic regions. It can begin at absolutely any age due to back injuries, a sedentary lifestyle, and overweight. An important role is played by hereditary factors and work in hazardous production (excessive vibration).
According to ICD-10, this type of osteochondrosis has a code M 42. 02.
Symptoms of cervicothoracic osteochondrosis include:
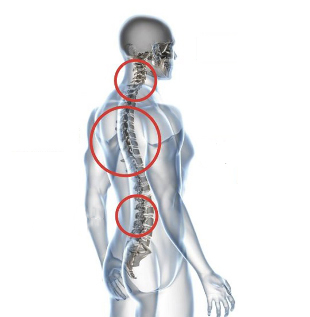
- Sudden dizziness.
- Aching pains in the neck and shoulders.
- Pain in the right hypochondrium.
- Blood pressure drops and tachycardia.
Osteochondrosis with radicular syndrome
The disease got its name due to the disruption of normal functioning in the roots of the intervertebral nerves.
When the roots are affected, a number of rather untidy symptoms develop, including sharp "shooting" pains in the lumbar region and neck.
Symptoms may also include:
- Short-term loss of ability to perform any movements.
- Loss of sensation in the limbs.
- Muscle hypotrophy.
- Changes in neurological reflexes (detected on examination by a neurologist).
The following factors are associated with the occurrence of radicular syndrome:
- Uneven load on the spine during overweight, pregnancy, wearing uncomfortable shoes.
- Asymmetry of the lower limbs, flat feet.
- Injuries, sharp loads on the spine.
If the disease is detected at an early stage, surgical intervention is not required.
Causes of cervical osteochondrosis

The main reasons for the development of osteochondrosis:
- Heavy weight and sedentary work, sedentary lifestyle.
- Previous spinal injuries and spinal curvature.
- Stress and nervous strain.
- Lack of physical fitness.
- Lack of healthy nutrition.
Degrees of osteochondrosis of the thoracic and cervical regions
In the development of cervical osteochondrosis, the following degrees of the disease are characteristic:
- For the first stagechanges in the intervertebral discs are characteristic. Changes begin to occur due to the disappearance of fluid reserves from the nucleus of the intervertebral discs. Pain is not yet noticeable.
- In the second stagethe intervertebral discs become flatter. As a result, there are strong loads on the ligaments and muscles, which, due to the constant strong load, begin to grow numb. Constant dizziness is characteristic.
- The third stageis characterized by significant changes in bone and cartilage tissues, the appearance of arthrosis.
- The fourth stageis characterized by the appearance of bone growths on the vertebrae.
Diagnostics
To diagnose osteochondrosis, the first step is to conduct a complete examination of the spine. Signs of osteochondrosis at the initial stage can be confused with a number of other diseases. It is necessary to carry out diagnostics by a highly qualified specialist.
To diagnose the disease, you need to contact the attending physician, who will refer you to a specialist of a narrower profile. The sooner a patient seeks medical help, the faster and safer treatment will be.

In fact, osteochondrosis is treated not by one specialist, but by several:
- Radiologist.After receiving the X-ray results, the picture of the disease will be clearer.
- Chiropractor. Determines the exact location and stage of the disease.
- The doctor is an osteopath.The treatment method is very similar to manual therapy.
- Physician - neuropathologist.Osteochondrosis is closely related to diseases of the nervous system. The doctor will help in the treatment of the disease, both in the first stage and in the second.
- Physician - physiotherapist.Is a specialist in physiotherapy exercises. Physical education helps only in the early stages of the disease.
A sharp exacerbation of the disease is considered quite common. In such cases, you should immediately consult a neurologist. Osteochondrosis of both the cervical, thoracic and lumbar regions is closely associated with nerve disease. The neurologist will prescribe a course of taking special medications that relieve pain.
Osteochondrosis during pregnancy and breastfeeding in women
Osteochondrosis during pregnancy is a common phenomenon, since during pregnancy a woman undergoes a global restructuring and a very strong load on the entire body. Disease on the fetus does not have any effect, but during childbirth it can cause a number of serious problems.
And the period of breastfeeding is also recommended to be observed by a doctor and to wear corrective corsets in order to reduce tension in the spinal column.
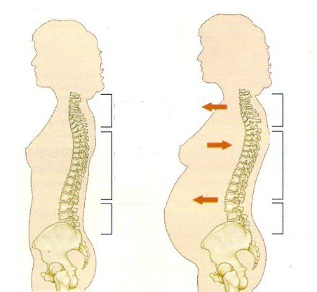
The reasons for the appearance of osteochondrosis during pregnancy include:
- Weight gain and severe stress on the spine and wearing uncomfortable shoes.
- Pressure of the uterus on adjacent organs.
- Change in hormonal levels.
- Deficiency of useful vitamins and minerals.
- Lack of rest and sleep, various kinds of stress.
To prevent the disease, you must consult a doctor at the first disturbing signs. You should not wait for the end of pregnancy. After childbirth, the disease can progress and it will be much more difficult to cure it.
If an illness is detected, the pregnant woman will be assigned to wear a prenatal bandage, a course of vitamins and minerals, as well as special gymnastics.
First aid for exacerbation of osteochondrosis at home
The duration of the exacerbation depends on the type and degree of neglect of the disease. Most often, an exacerbation can last from 1 week to 1 month.
Attention! In case of an exacerbation of the disease, it is prohibited: warming up in a bath, or any other heating, massage and self-treatment
If a sudden attack occurs, before the arrival of doctors, you must do the following:
- Provide the patient with maximum rest.
- If possible, lay the patient on a firm surface.
- Apply a cool compress to the affected area.
- Apply anti-inflammatory ointment to the affected area.
If a visit to a specialist in the near future is impossible, then you must resort to the following actions:
- Take a warm, relaxing shower.
- Do not make sudden movements.
- Don't lift weights.
- To avoid further pinching, keep the neck steady.
Dorsago and dorsalgia
Dorsagois the name of one of the symptoms of inflammation of the thoracic spine. Dorsago is characterized by sharp pains in the region of the heart, most often occurs in people doing monotonous seated work, or after a long stay in an uncomfortable position. With sudden movement, short-term breathing difficulties are possible.
Dorsalgiais a pain syndrome that occurs with a sharp exacerbation of the disease, lasting about 2 weeks. With dorsalgia, pain sensations increase gradually. The pain is especially severe when bending forward or deep breathing. Most often, pulling pains occur in the area of the shoulder blades, lumbar region.
Methods for the treatment of cervical and thoracic osteochondrosis
In case of a disease, various methods of treating osteochondrosis are used.

The most common are considered to be:
- Physiotherapy- paraffin compresses, magnetic therapy, laser therapy.
- Physiotherapygymnastics and massage.
- Reflexotherapy- treatment is carried out using needles acting on the affected areas. Before starting treatment, it is necessary to consult a specialist, since there are a number of contraindications.
- Folk remediesand diet.
- Medication- is prescribed only after a complete examination by a specialist.
Medication
To relieve pain in the spine, most often, doctors prescribe medications. When the stage is advanced, medications relieve pain for a short time. Therefore, to relieve pain and further inflammation, doctors prescribe NSAIDs in the form of tablets or capsules.
Chondoprotectors- another type of medication prescribed for osteochondrosis. The drugs are designed to protect and strengthen bone and cartilage tissue from destruction.
In case of a strong inflammatory process that occurs in muscle tissue, the patient will be prescribed drugs to relieve muscle spasms.
The dosage must be determined by the attending physician. The course of taking drugs is not more than 3 weeks.
Also one of the effective methods of drug treatment is the use of injections that can relieve pain.
Fixing means
In case of complex treatment, the patient may be prescribed to wear special fixing corsets and bandages.
Exercises for osteochondrosis
Exercises prescribed in a physiotherapy room can not only relieve pain, but also strengthen the muscles of the spine, which further prevents the development of various complications. And also after several courses of physiotherapy exercises posture significantly improves.
The famous doctor Bubnovsky has developed a set of exercises for the treatment of osteochondrosis, which can be used at home.
The most common exercises are:
- Walking, raising arms and legs smoothly.
- Rotation of the shoulders in different directions, bringing and extending the shoulder blades.
- Slow head bends to the side.
- Stretching exercises for the muscles of the spine and neck.
- Flexion of the arms and legs.
In case of cervical osteochondrosis, it is forbidden to rotate the head, as it is possible to provoke a complication of the disease.
Physiotherapy treatments
Physiotherapy is primarily aimed at reducing pain in the spine. The procedure improves blood circulation, enriches muscles with oxygen.

Today, the most common physiotherapy procedures are:
- Massage with vibration- helps to get rid of pinched nerves in the intervertebral discs. Contraindication - pregnancy, high blood pressure.
- Acupuncture- relieves pain. It also helps to relax your back muscles. A contraindication is epilepsy.
- Electrotherapy- the method consists in using a weak effect of current on the affected areas of the spine. A contraindication is the presence of heart disease.
- Ultraviolet- enriches the body with vitamin D, thanks to which calcium is absorbed more quickly. It also has an anti-inflammatory effect on the affected area. Contraindication to the procedure is the presence of blood diseases, allergic reactions on the skin, cancer.
Treatment of osteochondrosis with folk remedies
In the complex treatment of the disease, some doctors also recommend the use of folk remedies to eliminate the disease. In complex treatment, it is especially important to observe the correct dosage and method of treatment.
Folk remedies for home use relieve pain in the area of muscles and joints, and also restore joint mobility:
- Fir and turpentine ointment.150g. melt any fat of animal origin in a water bath 1 tbsp. fir oil and turpentine. After 20 minutes, remove the ointment from the heat, allow to cool and apply exclusively to the affected areas of the spine.
- Mustard compress.Combine mustard powder, vodka and camphor alcohol in equal amounts. After mixing well add 4 egg whites. Let the mixture brew for 4 hours. Apply a compress to the affected areas.
- Turpentine bath.Shake the solution vial thoroughly. Then pour 5 ml of emulsion into a warm bath. In subsequent times, the solution can be increased to 10-15 ml. You need to spend 20 minutes in such a bath. The water temperature should not exceed 40 degrees. It is also necessary to ensure that the water does not reach the heart area.
Method of osteochondrosis treatment according to Valentin Dikul
This technique is quite common in the treatment of the disease. Valentin Ivanovich Dikul, first of all, tested his method on himself. Dikul's technique is indicated for diseases of the spine and intervertebral hernias.
The following principles should be adhered to while exercising:
- Compliance with the order of the exercises.
- Gradually load the body with exercise.
- Regular performance.
- Exclude fast exercises, the technique implies smooth and slow movements.
Principles of nutrition for osteochondrosis

In case of complex treatment, a special diet must be followed, which includes:
- Drinking plenty of water.
- Adequate amount of vitamins and minerals in food.
- Eating foods rich in protein and calcium.
The diet assumes an exception:
- Fried, fatty and spicy foods.
- Refusal of quick snacks (sandwiches, fast food).
- Avoid eating a few hours before bed.
Preventive measures
To prevent the development of the disease, or to stop its development, it is necessary to use the following prophylaxis:
- Always monitor your posture, do yoga or do morning exercises.
- Limitation of sharp loads on the spine.
- Limit jerky movements.
- Avoiding uncomfortable shoes, as well as shoes with high heels.
- Equal distribution of the load on the spine when performing any work.
Conclusion
With proper observance of all the above recommendations, as well as with timely referral to specialists, almost any disease can be cured. Treatment of osteochondrosis takes much more time and money, but an advanced disease can lead to a wheelchair.



































